Physiotherapy for Hip Osteoarthritis: Symptoms, Causes, and Treatment in Burlington
- Folarin Babatunde PT PhD

- Jul 25, 2025
- 4 min read
Updated: Oct 31, 2025
Cogent Rehab Blog
Folarin Babatunde PT PhD MScSEM MScPT BScPT
July 25, 2025
What Is Hip Osteoarthritis?
Hip osteoarthritis (OA) is a degenerative joint condition where the protective cartilage covering the hip bones gradually wears away. As cartilage thins, the bones rub together, causing pain, stiffness, and reduced mobility. (Arthritis Society of Canada)
According to the Arthritis Society of Canada, hip and knee osteoarthritis are among the most common causes of disability in adults over 55. However, hip OA can also affect younger adults, especially those with a history of hip injury, repetitive loading, or genetic predisposition.
Anatomy of the Hip Joint
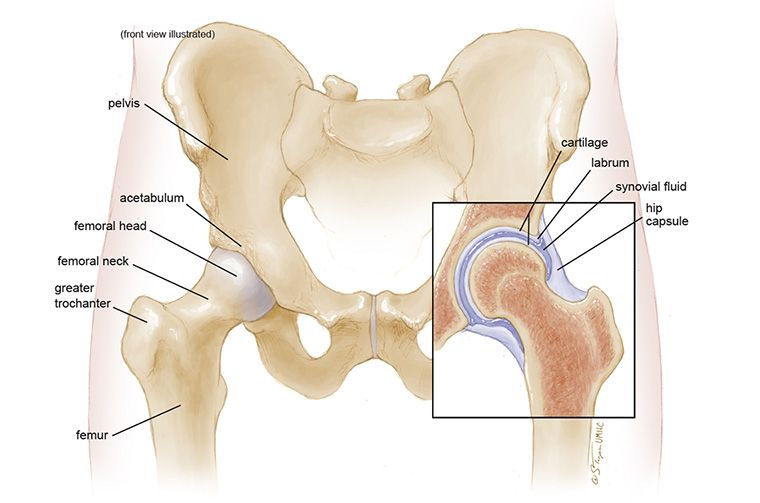
The hip is a ball-and-socket joint, one of the largest and most stable joints in the body. It includes:
Femoral head (ball): the rounded top of the thigh bone
Acetabulum (socket): a curved part of the pelvis that houses the femoral head
Cartilage: smooth tissue that cushions and allows friction-free movement
Ligaments and capsule: stabilizing structures that hold the joint together
Muscles around the hip: including gluteal muscles, hip flexors, and adductors, which allow motion and support the joint
In hip OA, cartilage breakdown leads to inflammation, bony spurs (osteophytes), stiffness, and progressive loss of function.
Learn more about how we support recovery through Orthopaedic Physiotherapy in Burlington.
Signs and Symptoms of Hip Osteoarthritis
Hip OA symptoms typically develop gradually. Some of the most useful clinical findings that may point to hip OA include:
Groin pain when the hip is moved outward (abduction) or inward (adduction)
Weakness of the hip abductor muscles (often noticed as a limp or difficulty lifting the leg sideways)
Decreased hip movement — especially in inward (internal) rotation or adduction
Stiffness after resting, especially in the morning
Reduced hip mobility, particularly in internal rotation and adduction
Pain at the back of the hip when squatting

Hip OA is less likely if passive hip adduction (inward movement of the leg without muscle effort) is normal. For other causes of hip discomfort, visit our Hip & Thigh Pain page.
Causes and Risk Factors
The exact cause of hip OA is often a combination of factors. The most common include:
Age: risk increases with age
Genetics: family history of OA
Previous injury or surgery: hip fractures, dislocations, or labral tears
Obesity: excess weight increases stress on the hip joint
Repetitive stress: high-impact sports, occupational loading
Structural conditions: hip dysplasia or femoroacetabular impingement (FAI)
Treatment Options for Hip Osteoarthritis
Conservative (Non-Surgical) Management
Physiotherapy: the gold standard and first-line treatment (OARSI Guidelines, 2021). Physiotherapy helps restore mobility, reduce pain, and improve function.
Exercise therapy: strengthening, stretching, and aerobic conditioning programs tailored to the individual.
Lifestyle adjustments: activity pacing, weight management, footwear changes.
Pain relief: physician-guided use of medications, injections, or modalities.
Learn how we use movement-based rehab strategies through our Sports Movement Rehabilitation services.
Surgical Management
When conservative care no longer provides relief, hip replacement surgery may be considered. This procedure replaces the damaged joint surfaces with artificial components and is highly effective in restoring mobility. Prehabilitation (physio before surgery) and post-surgical rehab both improve outcomes.
Our Neurological Physiotherapy programs also support gait retraining and mobility for hip OA patients.
Why Choose Cogent Rehab in Burlington?
At Cogent Physical Rehabilitation Centre, we provide comprehensive, evidence-based physiotherapy treatment for patients with hip osteoarthritis. Here’s why patients choose us:
Expertise: Our team has advanced training in musculoskeletal rehabilitation, chronic disease management and sports medicine.
Evidence-based treatment: We follow the latest international guidelines, ensuring your care is backed by research instead of guess work.

Physiotherapist treating hip osteoarthritis with manual therapy in Burlington Personalized care plans: Every program is tailored to your goals, whether that’s walking pain-free, returning to sports, preparing for or recovering from hip replacement surgery.
Continuity of care: From early-stage management to pre- and post-operative rehab, we support you through every phase of recovery.
Community focus: As a Burlington-based clinic, we’re dedicated to rebuilding, promoting, and enhancing recovery for our local residents in Burlington and the Halton region of Ontario.
Ready to take the next step with physiotherapy for hip osteoarthritis in Burlington? Contact Cogent Rehab Burlington today to book your appointment.
Take the Next Step
Hip osteoarthritis is a common but manageable condition. Hip osteoarthritis doesn’t have to limit your life. With expert physiotherapy and evidence-based care, you can reduce pain, restore movement, and stay active.
Cogent Physical Rehabilitation Centre – Find us at 3077 New Street, Suites 300-302, Burlington, ON
Frequently Asked Questions (FAQs) About Physiotherapy for Hip Osteoarthritis in Burlington
1. What are the first signs of hip osteoarthritis?
The earliest symptoms are usually groin pain, stiffness in the morning, and difficulty with activities like squatting or climbing stairs.
2. Can hip osteoarthritis be reversed?
No — the cartilage loss in your hip cannot be reversed, but physiotherapy can slow disease progression, reduce pain, and improve function.
3. When should I see a physiotherapist for hip OA?
If hip pain or stiffness lasts more than 2–3 weeks or affects your ability to walk or perform daily activities, you should make an appointment to see a physiotherapist.
4. Do I always need surgery for hip OA?
Not necessarily. Many patients successfully manage their symptoms long-term with physiotherapy and lifestyle strategies. Surgery is a last resort when pain and disability remain severe despite conservative care.
5. How does Cogent Rehab treat hip OA differently?
We combine manual therapy, mobility retraining, and individualized exercise programs. Our team also supports pre- and post-surgical patients to maximize recovery.
Sources
Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip and polyarticular osteoarthritis. Osteoarthr Cartil Open. 2019;27:1578-1589.
Sabha M and Hochberg MC. Non-surgical management of hip and knee osteoarthritis; comparison of ACR/AF and OARSI 2019 and VA/DOD 2020 Guidelines. Osteoarthr Cartil Open. 2021;25:100232.
Lespasio MJ, Sultan AA, Piuzzi NS, Khlopas A, Husni ME, Muschler GF, Mont MA. Hip osteoarthritis: A primer. Perm J. 2018;22:17-084
van Doormal MCM, Meerhoff GA, Vliet Vlielan TPM, Peter WF. A clinical practice guideline for physical therapy in patients with hip or knee osteoarthritis. Muscl Care. 2020;18:575-595.



Comments